REVIEW ARTICLE
GDP Growth and Health Care Expenditures Worldwide
Milos Stepovic1, *
Article Information
Identifiers and Pagination:
Year: 2019Volume: 7
First Page: 9
Last Page: 18
Publisher Id: TOPHARMEJ-7-9
DOI: 10.2174/1874129001907010009
Article History:
Received Date: 17/05/2019Revision Received Date: 27/06/2019
Acceptance Date: 08/07/2019
Electronic publication date: 30/08/2019
Collection year: 2019
open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Impact of large recessions on GDP growth is well documented and their effect on Gross Domestic Product (GDP) growth is definitive. Health care expenditure is growing everywhere in the world. The most important factors such as GDP, income per capita, health system factors, urbanization, aging, and socio-demographic factors are well determined and described.
Objective:
The main aim of this literature review is the summation of all factors affecting the GDP and healthcare expenditure. The second aim is presenting the bigger picture of the multifactorial connection between all impacts on healthcare expenditure. The last aim is proposing possible strategies for the development of sustainable health systems.
Conclusion:
Tracking the economic trend changes is necessary. Government investments in health must be as large as countries can afford due to the population aging, non-communicable disease and treatment, and pharmacological innovations. The cost-effectiveness estimates and Hierarchical task analyses are among some plausible solutions for making informed resource allocation decisions.
1. INTRODUCTION
Healthcare expenditure is growing in all countries. Healthcare expenditure is becoming a significant challenge for the financial sustainability of national health systems even in high-income countries. Both developing and developed countries are working to define the factors involved in this healthcare expenditure management. Indicators affecting economic growth can be tracked ever since the largest recessions. Understanding economic growth concept is essential in order to point out cross-country variation in adaptable policies and mistakes, especially in the time of crisis. Literature data determined some factors related to healthcare expenditure: income per capita as the core one, health system factors, GDP, socio-demographic characteristic (gender and age), and level of urbanization. The problem of healthcare expenditure is multifactorial. Healthcare expenditure management differs not only in different areas in the world but also in different parts of the same country. For instance, per capita spending, as well as GDP allocation percent is different in developing and developed countries, which is managed by financial and political decisions.
The first aim of the study is to review the existing literature focusing on GDP and health expenditure growth. The second aim is to assess the existence of the relationship between them. Firstly, the paper is making an overview of the historical effects of the biggest recessions in the world on GDP and recovery of countries. Secondly, it reviewed papers dealing with the subject of the health care expenditure of OECD, BRICS, CEMAC, CIVETS, MENA, and countries which are not part of these clusters. In the end, this paper summarized all the available knowledge of crucial factors influencing health care expenditure in relation to GDP growth. This literature review provides a narrow focus on existing knowledge gaps that will initiate some future research. Also, it gives a hint on plausible government strategies that may be crucial for the development of sustainable health systems.
1.1. Historical Effect of Large Recessions on GDP
An economic recession is defined as a decline in GDP for two or more consecutive quarters. If the recession affects multiple countries and lasts for a long time, then it is defined as a deep recession [1, 2]. A lot of macroeconomic indicators are used to compare recessions like – GDP decrease, personal income, trade volume decrease, increase in the unemployment rate, duration, etc. [3, 4].
The most severe recession (1929-1939) was the Great Depression. It started in the US but affected every country in the world with different severity. It lasted for one decade. Recession in Latin America and Germany started in 1928. Although it started a little earlier than the US recession, it made an almost equal loss [5, 6]. There were a lot of factors acknowledged as a cause for recession but the main problem was government policies. This depression resulted in increased unemployment rates and big declines in output [7, 8]. Between 1929 and 1933, industrial production in the US decreased by almost its half, the GDP by one third, and the unemployment rate increased by twenty percent. GDP growth in this period was slower than before the First World War [9, 10]. A lot of countries experienced negative economic growth. Considering economic growth, the leading countries were Canada, the US, Austria, Netherlands, New Zealand, Germany, and France. Countries afflicted by banking and financial crises were Austria, Belgium, Estonia, Finland, France, Germany, Hungary, Italy, Latvia, Norway, Poland, Romania, Switzerland, United States, and Yugoslavia [11]. Trade declined in 27 leading countries during this period [12]. The UK had a low growth rate during most of the 1920s because of their decision from 1925 to return to the gold standard. The depression in the UK and France officially started in 1930. However, the decline in industrial production in the UK was not as severe as in the US though it was still considerable [13, 14]. Some less developed countries also experienced severe depressions. Argentina, Brazil, and Japan had been afflicted with an intermediate depression level [15, 16]. The US recovery began in 1930 with a GDP rise of about 9% and finished in 1942 when the US was on track with the previous trend position. The economic recovery of the UK, Latin America, Germany, and Japan started at a similar period, during 1932 [17]. Canada and Europeans countries started to recover after 1933. France was an exception because of her later depression experience. France started to recover in 1938. [18]. The biggest economic impact of the Great Depression was an alarming rate of unemployment [19]. GDP is eventually restored over time but slumps after a recession last for a long time [20].
A very important recession occurred during the 1970s. Its importance and the main difference in relation to other recessions was the coexistence of high infiltration and slow economic growth and the high level of unemployment rates. This crisis affected Europe and North America mostly due to their competitiveness in the rising metal industry. The crisis becomes obvious after the stock market crash in the UK followed by a decrease in GDP and electricity deliver [21].
The decrease in GDP during this period was not the main concern. The main concern was high and constantly rising unemployment rates. The low unemployment rate from before the crisis has never been restored after the recession [22]. The oil crisis which started in the Middle East when the price of oil increased was considered to be the cause [23].
The economic collapse of post-Soviet Republics in 1990 was followed by two of the biggest recessions: recession in Russia and recession in Ukraine. During the recession in Russia (1991-1996), GDP declined to nearly its half, mostly in military-industrial production [24]. Ukraine experienced an even worse economic breakdown (1991-1999) with GDP in 1999 being only 40% of GDP in 1991. Recessions in both countries were classified as ultra-recessions [25 - 27]. Concerning the Asian financial crisis (1997-1999), recession in Thailand was disastrous. Japan experienced two smaller recessions. Recession in South Korea was classified as major [28]. An Argentinean recession (2001-2002) was considered to be severe, with the decline of GDP growth rates to 4.04%, especially in time of the largest economic decrease when GDP decreased by 10.9% in one year [29].
Among the Scandinavian countries, Finland experienced the biggest recession after 1995 and again in 2008 and 2009. The low growth period in Denmark (1980) was not as bad as recessions in Sweden and Finland (1990) [30]. Recovery courses after these recessions were different. Sweden recovered the fastest. In 2010, the annual growth of GDP in Sweden was near 6%. The other two countries recovered but much slower. Difference between crises in 1980 and 1990 and the crisis in 2008 and 2009 was the lower unemployment rate in the latter. This difference could be explained by the adjustment of Nordic countries to the crisis- They used temporary changes, not permanent ones [31].
The global financial crisis, which started in the USA in 2007, can be considered as a major recession in the EU and Japan and a severe recession in the USA [32]. 25 of 27 EU countries experienced a recession (except Poland and Slovakia). The strongest recession was in Latvia and Estonia and the weakest in Cyprus, Malta, and France. In 2010, all major economies restored to the initial growth rate except the European. European economy got into a new recession in 2012. By data on GDP, it affected mostly small or medium-size countries [33, 34].
BRICS, the association of five major emerging national economies: Brazil, Russia, India, China, and South Africa, conducted viable health reforms in recent years. Health reforms of BRICS were diverse but they shared a common aim – the strengthening of the government’s role in health and financing health care. Reliance on public financing is necessary for universal health coverage. However, private financing, in the form of voluntary health insurance and OOP (Out-of-Pocket), represents a large part of health spending. BRICS spend less total government spending on health than many OECD countries. There were different motives for reaching the UHC (Unified Health Care) health insurance system in BRICS. Due to the fact that rail had been under military influence for a long time, there were tendencies for health reforms to be driven rather by civil society than government. So, in 1988, a Unified Health System was established. There was universal health coverage in the Soviet health system but such coverage collapsed with the break-up of the Soviet Union. The early post-Soviet health reforms of 1990 introduced mandatory health insurance. Universal health coverage is now guaranteed in the Russian Federation. In India, several factors led to the health reforms. The existing public sector system by which it was expected to deliver low-cost health care to all Indians failed and out-of-pocket payments placed a large burden on the poor. In 2005, the reforms of health care in the public sector took place. National Rural Health Mission and National Urban Health Mission were intoduced. In China, health insurance coverage was far from universal. By 2002, only about half of the urban population and 90% of the rural population had insurance coverage. Reforms that were made in 2009 gave the Chinese government a major role in the health sector, adjusting public funds to increase insurance coverage and strengthen primary care services. In South Africa, where non-communicable and communicable disease and injuries affected lower socio-economic levels, low percent of the population had private insurance and the majority relied on tax-funded services. Due to that fact, the South African government introduced a tax-funded National Health Insurance Fund as the solution for future UHC.
Due to the fact that universal or near-universal health insurance coverage exists in most OECD countries, coverage extension has been the focus of recent reforms in only a few countries. Australia, for example, shifted from a voluntary to mandatory universal insurance with the introduction of Medicare in 1984. Switzerland mandated the compulsory purchase of a private health insurance policy in 1994, with that moving from near-universal to universal coverage. Since establishing its social health insurance program, Spain has implemented a series of coverage expansions. By 2000, coverage reached 99.8% of the population. France filled the final gaps in social insurance coverage in 2000, by its Couverture médicale universelle. In the Netherlands, insurance has been made compulsory for 65% of the population, including all vulnerable groups.
Lack of coverage for certain services such as dental care, prescription drugs, mental or behavioral health care, rehabilitative or post-acute care, and infertility treatments vary widely across OECD countries. Korea, Mexico, and Turkey have systems in which more than a third of the cost is borne directly by patients. The practice of patients making out-of-pocket payments to supplement provider fees is common in a small number of OECD countries (mainly among the new Eastern European members).
Lack of health insurance coverage in America is a significant threat to the overall wellbeing of their citizens. Health care in America is one of the most expensive in the world. Also, it is one of the few without universal health coverage. Reforms suggested by the country’s leaders in 1912, 1932, 1948, and 1971 were taken down by the American Medical Association. In fact, for many years, the AMA was a leading opponent of universal health care until the American Counseling Association in 2010. The most significant change was brought by LB. Jonson in 1965. Although it had not presented universal health care, it covered people who were less likely to have health insurance, such as older adults, the disabled, and poor children. Today, nearly 90% of Americans have health insurance. The ACA has had its successes, but also its challenges. With the rising costs of health care and poor population health outcomes compared to other high-income countries, more reforms will be needed soon.
Recessions are of great importance because they describe the periods when countries had to adapt and change their health system priorities. The recession affected the micro and macro-economics of every country so the Government had to adapt their investments in public health sectors. Adaptation had not always been made properly. Mistakes that the Governments made affected the tempo of economic recovery. Understanding the historical background of economic recessions is essential in order to prevent it from repeating. Also, it is crucial to make an unbiased revision of governmental impact on great economic recessions of the past. That will give health economy researchers an insight which will instruct them to form and propose more efficient strategies in health expenditure management.
2. METHODS AND EARCH STRATEGY
This paper represents a descriptive literature review of articles dealing with the subject of GDP and HCE growth. Analyzed articles are not country-specific; they included all representable conclusions from developing and developed countries with reference to OECD, BRICS, CEMAC, CIVETS, and MENA countries. An electronic search of the published literature was conducted in NCBI Databases — MEDLINE /PubMed, NLM Catalogue, and PubMed Central using a combination of keywords by which we got the articles we considered in our paper (Fig. 1). Also, Google Scholar and World of Science were used for additional search.
Inclusion criteria were full-available articles in English, original articles, data report, and review articles not older than 20 years. Exclusion criteria were articles not fully available, unpublished studies, studies older than 20 years, and studies with no interest in the subject of GDP and HCE.
Electronic searches were conducted with the last year of 2018. The applied combination of keywords was carefully chosen to cover the most commonly used terms in the titles of publications dealing with global domestic products and health care expenditure. We tried to ensure inclusion of the largest possible number of the publications dealing with health economics, and exclusion of the largest possible number of irrelevant publications. No filter was applied in the MEDLINE database. The final applied combination included keywords combined with the Boolean search operators “OR” and “AND.”
The next combinations of keywords were used with the purpose of getting the information of importance for the subject of the paper’s interest: health care expenditure and developing countries, health care expenditure and developed countries, GDP and developing countries, GDP and developed countries, GDP and health expenditure, health care expenditure and health care system factor/income/socio-demographic factors/urbanization.
After a detailed search, only articles dealing with the problem of healthcare expenditure and GDP growth were taken into consideration. Summation of all results can be found in Table 1.
| Year | Authors | Type of Study | Country | Relationship* |
|---|---|---|---|---|
| 2016 | Jakovljevic | Commentary article | Japan | Yes – Elderly and HCE |
| 2016 | Jakovljevic and Getzen | Data Report | Low and middle income country, BRICS, N-11 | Yes – GDP and THC |
| 2014 | Rao et al. | Original article, Cross-sectional | BRICS | Yes – GDP and health care |
| 2001 | Hashmati | Original article, Cross-sectional | OECD | Yes – GDP and HCE |
| 2002 | Gerdtham and Lothgren | Original article, Cross-sectional | OECD | Yes – GDP and HCE |
| 2013 | Lago-Peñas | Original article | OECD | Yes – Per capita income, GDP and HCE |
| 2012 | Elmi and Sadeghi | Original article | Developing countries | Yes – Income and GDP |
| 2017 | Cetin and Ecevit | Original article, | OECD | Yes – GDP and HCE |
| 2015 | Ollivaud and Turner | Review article | OECD | Yes – Global crisis and GDP |
| 2017 | Kouki et al. | Review and original article | Emerging and developed countries | Yes – Financial crisis and GDP |
| 2014 | Majdi and Younes | Data report | Developed, emerging, and countries in development |
No – Crisis and GDP |
| 2017 | Zaman et al. | Data report | Bangladesh | Yes – GDP, income and HCE |
| 2012 | Eryiğit et al. | Original article | Turkey | Yes – Education, HCE and economic growth |
| 2017 | Piabuo and Tieguhong | Review article | CEMAC | Yes – HCE and economic growth |
| 2011 | Mehrara and Musai | Original article | Oil exporting countries | No – GPD and HCE |
| 2017 | Ali et al | Original article, Panel study | Pakistan, China, India, and Bangladesh | No - Health expenditure and GDP |
| 2016 | Wouters and McKee | Review | OECD | Yes – HC and private funding |
| 2013 | Yi et al. | Original article, comparative analysis | CIVETS | Yes – Economics growth |
| 2016 | Akadre | Original article | CIVETS | Yes – Economics growth |
| 2006 | Le et al. | Original article | Vietnam | Yes – Private sector development and economic growth |
| 2015 | Tomé, and Goyal | Original article | India | Yes – Human resource development, education, and economic growth |
| 2013 | Sghari and Hammami | Original article | Developed Countries |
Yes – Bilateral causality GDR and HCA |
| 2016 | Bedir | Original article | Developing countries | Yes – Income, GDP and HCE |
| 2007 | Collier and Goderis | Original paper | Developed and developing countries | Yes – Income and HCE |
| 2012 | Mehrara et al. | Original article, Panel study | MENA | Yes – HCE and GDP |
| 2007 | Costa Font and Pons Novell | Original article | Spanish region | Yes – Insurance and HCE |
| 2009 | Mehrdad | Commentary article | Iran | Yes – Health system and HCE |
| 2016 | Rezaei et al. | Original article | Iran | Yes – GDP per capita, degree of urbanization, illiteracy rate and HCE |
| 2012 | Magazzino and Mele | Original article, Panel study | Italy | Yes – GDP, unemployment rate, the number of beds in community hospitals, urbanization, % of the population and HCE |
| 2011 | Bilgel and Tran | Original article, Panel study | Canada | Yes – GDP, urbanization and HCE |
| 2014 | Jakovljevic | Commentary article | Serbia | Yes – GDP growth |
| 2014 | Jakovljevic | Original article | BRICS | Yes – Insurance and HCE |
| 2011 | Jakovljevic et al. | Original article | Serbia | Yes – HCE growth |
| 2013 | Jakovljevic | Review article | Southeastern Europe | Yes – HCE studies and HCE growth |
| 2016 | Jakovljevic et al. | Original article | Eastern Europe | Yes – GDP and HCE growth |
| 1989 | Kim and Chun | Original article | Korea | Yes – Increase in hospital bed, degree of urbanization and HCE |
| 2002 | Lee and Jung | Original article | Korea | Yes – Population size, elder population, number of physicians and HCE |
| 2004 | Tchoe et al. | Original article, Panel study | Korea | Yes – GDP, elderly and HCE |
| 2012 | Squires | Original article | United States | Yes – Higher prices, more accessible technology, and HCE |
| 2013 | Kimyoung et al. | Original article | Korea | Yes – Elderly population, GDP and HCE |
| 2006 | Leal et al. | Original article | European Union | Yes – Noncommittal diseases and HCE |
| 2014 | Fanourgiakis and Kanoupakis | Original article | European Union | Yes – Noncommittal diseases and HCE |
| 2015 | Petrou | Original article | Cyprus | Yes – Number of emergency room visits, number of unnecessary laboratory tests and HCE |
| 2014 | Petrou | Original article | Cyprus | Yes – Pharmaceutical expenditureand HCE |
| 2017 | Abdullah et al. | Original article | Asia | Yes – Income and HCE |
| 2014 | Lv et al. | Original article | African | Yes – GDP, income and HCE |
| 2008 | Clemente et al. | Original article | OECD | Yes – Non-pharmaceutical expenditure and HCE |
| 2019 | Dinçerand Yuksel | Review article | E7 countries | YES – Economic growth and HCE |
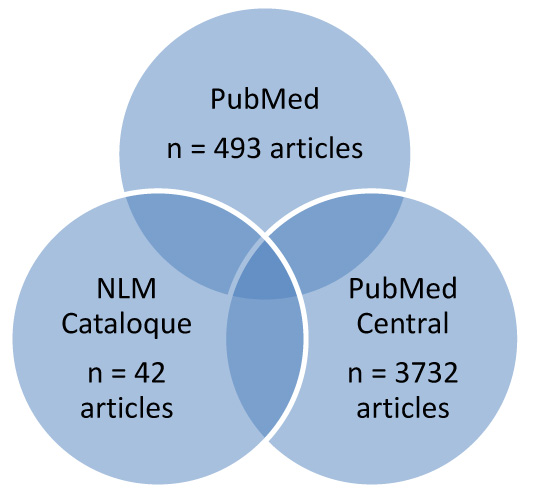 |
Fig. (1). Number of found articles in named databases. |
3. REVIEW OF THE LITERATURE ON HEALTH EXPENDITURE AND ECONOMY GROWTH
Total health expenditure is defined as the sum of public and private health spending and it covers both the preventive and curative services along with emergency and rehabilitative health services for the entire population. Ministry of Finance of a country allocates the budget for health expenditure in a fiscal year. That allocated budget has been reported by different studies to differ for developed and developing countries [35]. The relationship between public health expenditure and economic growth has been investigated in developing and developed countries, but researchers have not come to a general conclusion. This may imply that healthcare expenditure will mostly be managed by private insurance and out-of-pocket payment. With that, growth of the total health expenditure has become an immense concern in most of the developing countries as along with out-of-pocket spending, especially in third world countries [36].
One of the biggest and latest global financial crises was widely known as the Subprime mortgage. In European countries, as well as the United States, the financial crisis caused by the mortgage crisis was serious. European Central bank decided to lower the rate of interest taken in 2008 as the first act against newly formed crises. Japan was also a victim of great depression 2008-09. Japanese manufacturing industries such as the auto industry had fallen into a slump. In 2007, international sale of automobiles had exceeded domestic sales but in 2008-09, some of the contract workers were cut off. Japan was not directly involved in the subprime mortgage crisis, but its economy depended on external demand and, therefore, it was negatively affected. A lot of US investors withdrew a huge amount of money from the BRICs stock market, which caused the shrinkage of the stock market index in each of the BRICs. It was particularly obvious in Russia and Brazil. But BRICs are now facing a different stage, and the economy of each of its countries is close to the mature mode. The number of people in upper-income brackets increased recently and their domestic demand is going to spread. Despite a global financial impact, India can achieve a 7-8% growth rate in the forthcoming years. Its economy will be more under the control of domestic than international factors. In 2008, China announced to take measures to counter depression supervised by their government. They ought to help in trade and regaining the Chinese market credibility. In the end, BRICs total GDP based on PPP share of world total exceeded the US’s in 2007. BRICS countries relevance refers to the fact that they are the core of the EM7 group and contribute mostly to one half of the real economic growth worldwide. Furthermore, their potential for improvement in universal health coverage by extending health care investment remains substantially larger in comparison to most high-income OECD economies. This is due to large surplus and economic growth and significant existing inequities. A large share of the general population is still living beneath or close to the poverty line. In the study about evolving healthcare expenditures of BRICS countries, Jakovljevic et al. found that these countries were able to increase their investments in health care but with the increase in the out-of-pocket share of health spending. Russia’s per capita spending was the highest in 2013 and by the statistics, this will not change in the future. In the future, China will increase its percentage of GDP spent on health care [37]. India and South Africa have the advantage of younger populations and Russia and China have a problem of increasing trend in population aging [38]. Existing health care sectors in the BRICS economies may not be enough to meet rising population demand for medical services. Due to the fact that BRICS countries are considered to be high and middle-income countries, the out-of-pocket share of health spending is an important part of healthcare expenditure. Nevertheless, Out-of-Pocket healthcare spending can harm the house’s budget [39 - 42].
Using data from 25 OECD countries, Gerdtham et al. found the correlation between health expenditure and GDP [43]. Researching OECD countries by Solow growth model, Hashmati found a positive connection between HCE and economic growth. A study conducted by Elmi and Sadeghi also found a positive connection between HCE and economic growth. Cetin et al. found a negative correlation between HCE and economic growth [44-45]. In the research conducted by Ollivaud et al., 19 OECD countries experienced a banking crisis from 2007 to 2011 with big losses in output. Bad resource allocation is identified as the main reason [46]. Lago-Peñas’s results based on data from 31 OECD countries showed that HCE is more sensitive to per capita income than to trend movements [47].
In a study of 17 emerging markets and 11 developed countries over a period of 31 years, Kouki et al. found that financial crises have negative and significant effects on economic growth and that developed financial system can reduce crisis [48]. Research of Ksantini et al. on a panel of 25 countries over the 12 years showed that the duration of the crisis depends on the state of development of countries and type of crisis. The financial crisis in the US in 2007 caused an economic slowdown in all regions of the world with the biggest effects on emerging and developing countries [49].
Zaman et al. analyzed the data from Bangladesh, where income had a direct influence on health spending at the individual level. They found a direct relationship between GDP and total HCE [50]. In some studies concerning healthcare expenditure in Turkey, the correlation between economic growth and health expenditure was positive and in some was negative [51].
Results from Piabuo showed that health expenditure has a positive and significant effect on economic growth in both CEMAC countries and five African countries [52]. A lot of studies from Asia and Latin America confirmed that the economic and financial crises resulted in cuts in expenditures on health, lower utilization of health services and health outcome. Monitoring financial situation in Africa is necessary for its health sector protection [53]. The total GDP in the African Region shrunk by 8.6% between 2008 and 2009. The decrease in GDP per capita was the biggest among oil-producing countries.
Ali et al. analyzed four developing countries of Southeast Asia - Pakistan, India, China, and Bangladesh. They got to the conclusion that these countries were struggling in maintaining the quality of health services. GDP of Pakistan, India, and Bangladesh had increased, but of China decreased. China and India are considered to be adequately managing health expenditure. On the other hand, available data indicate Pakistan and Bangladesh need to pay a lot of attention to the development of their health sector. In Southeast Asia, the effect of health expenditure on GDP was insignificant [54]. Abdullah et al. investigated the relation between healthcare expenditure and income in Asian countries for a period of almost twenty years. They concluded that relationship exists and healthcare may be defined as necessary [55].
Since the global economic downturn in 2008, high-income countries cut public health care spending. In high-income countries, private health insurance models implementation will ensure larger health care insurance coverage. On the other hand, in low and middle-income countries there is a doubt that private or public-financing models, or a mix of those, are the best option for reaching for universal health coverage [56].
CIVET’s countries are among the biggest and fastest-growing emerging markets - accounting for more than 50 percent of the world's population, 40 percent of its total geographic area, and 50 percent of global GDP. In research by Yin et al., CIVETS have a lot of commonalities: increasing young population (average age 28), significant economic growth (average annual GDP growth of 4.5% until 2030), and suitability for foreign investment [57]. They are facing high unemployment, corruption, and inequality which are significant barriers for development. CIVETS are experiencing similar levels of economic growth as the BRIC nations in the past ten years. In the research of Akdere, it was found that all CIVETS countries had a big increase in annual GDP during the period of 2000-2012, especially India and Vietnam in 2012 [58]. Global Competitiveness Index ranked Indonesia on the highest place from other CIVETS countries [59, 60].
Ammar Sghari et al. analyzed the relationship between the HCE and real per capita GDP in developing countries (Australia, Austria, Belgium, Canada, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Japan, Korea, Luxembourg, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Republic of China, Slovak Republic, Spain, Sweden, Switzerland, Turkey, United Kingdom, and United States) from 1975 to 2011, highlighting dependence per capita GDP and per capita HCA from one another [61].
Bedir investigated the relationship between economic growth and HCE over the emerging markets in Europe, Middle East Africa, and Asia. He found bilateral causality for the Czech Republic and the Russian Federation. The evidence from Egypt, Hungary, Korean Republic, South Africa, and the Philippines supports the health view over the income view. The evidence from Greece, Poland, United Arab Emirates, China, Indonesia, and the Korean Republic supports the income view over the health view [62]. The general conclusion was that income is an important factor in explaining the variations in healthcare expenditures among countries [63]. GDP level defines the elasticity of income for health spending. The elderly population has effects on healthcare expenditure in African countries and healthcare is necessary good [64].
A portion of GDP used for health expenditure in developed countries is usually bigger than in the developing countries. When the level of development increases, health expenditures increase too. Mehrara et al. found that the share of GDP on expenditures decreases with GDP decrease which indicates that health care is not a luxury in MENA countries [65].
Health care system in Iran comprises from three sectors – a public one which is directed on the primary health care, not-for-profit one for chronic and severe patients, and private sector directed to secondary and tertiary health care. A study by Costa-Font et al. indicated that healthcare budget depends on private and public expenditures and type of healthcare financing [66]. In Iran, the share of HCE as a percent of GDP increased as well as the general GDP invested in healthcare from 2000 [67]. Rezaei et al. indicated three things that lead to a big increase in HCE - GDP per capita, urbanization, and literacy rate. Increase in the number of patients aged 65 and physicians decreases health care expenditures [68]. Other studies also suggest that GDP per capita and urbanization have a positive effect on HCE in Iran [69, 70].
National health care expenditure in Serbia followed the trends from the surrounding countries [71]. GDP increased from lower to the upper middle income in 2012 [72]. Jakovljevic et al. showed that a lot of the countries in Central and Eastern Europe had strong growth in national health expenditure. EU 2004, CIS, and SEE regions experienced differences in their healthcare reform with the strongest expenditure growth among EU 2004, SEE, and the CIS [73 - 76].
HCE expenditures in Korea are related to factors often investigated in the world - GDP, population size, elder population, and the number of physicians and medical institutions [77 - 79]. GDP per capita and population over the 65 years had the strongest effects on HCE [80]. This was also shown in the study of Han et al. where health spending was associated with the proportion of the elderly population (22.4%) and GDP per capita (4.5%) and with Medicare Economic Index in inverse association (-12%) [81].
In the systematic review of Dincer H, Yüksel S. that covered articles on the subject of HCE in E7 countries, it was clear that economic growth has a big impact on expenditure (total, public, and private). Increase in health expenditure positively affects economic growth but also the private health expenditures affect economic growth negatively. In emerging countries, governmental health expenditure is very big, much bigger than private. Recommendations are aiming at the improvement of the private sector role [82].
Noncommittal diseases are one of the reasons why health expenditures are increasing in all countries. In a macroeconomic level, the countries have costs from screening tests, diagnostic tests, medications, hospital, and others [83, 84]. Health spending can be very dramatic across countries with an income reduction, unemployment, and epidemics of chronic illness. Fanourgiakis et al. remind the fact that cardiovascular disease is the number one cause of death and in 2009, the EU estimated the costs of cardiovascular disease to be nearly 196 billion per year, which implies the necessity of financial measures to be taken by governments [85]. Cyprus is a unique case in the EU since it is the only country without a universal National Health System. Their current healthcare sector is divided into public and private. Due to poor cooperation between those two sectors, there had been an increase in costs. Petrou’s study indicates the necessity of reforms in health sectors such as a reduction in the number of emergency room visits and unnecessary laboratory tests as well as economic evaluation of pharmaceuticals [86, 87]. Governmental pharmaceutical expenditure is controlled by policymakers, but private pharmaceutical expenditures are in growth. That leads to total pharmaceutical expenditure growth. Clemente et al. showed non-pharmaceutical expenditure to be a significant reason for total HCE reduction [88, 89].
The entry of every country to BRICS is an effort to acquire benefits from the other members. Every country wants investments from others and the ability to utilize resources is something the BRICS nations have displayed more than other emerging markets. BRICS are moving in the right direction while implementing the best HRD practices. The developing nations that are still unable to compete are less willing to adopt HRD techniques. Reaching universal health coverage is an agenda of primary importance in each and every country worldwide. Investigations on this subject and comparison of the results and facts will lead to the huge importance in the way of readjusting of the health system and prioritization of the right problem. So far, the BRICS countries showed the hugest progress in these areas with space for more adjustments and the next eleven countries and OECD are not far behind.
CONCLUSION
After the huge historical recessions, most countries worldwide experienced contractions in their disposable GDP. Through years, some of them successfully solved the problem, faster or slower. The latest 21st-century global recession was not discriminating. It hit every country in the world. Some of them are still recovering. There had always been differences between low and high-income countries in the speed of recovery. Some of the major problems were: the type of country’s health system establishments, health care financing and provision, and the percent of GDP invested in the health. Non communicable diseases are rising in prevalence. Population aging is accelerating as well as the unemployment rates that differ in the countries in the world. There is no universal solution for the problem of economic output decrease. Individual strategic approaches are the best way. Trends in economics must be tracked constantly so the problems can be seen in time and through budgetary cuts and savings may be prevented to some extent. The scale of total investment in healthcare should be as large as the countries can afford because of the population aging and non-communicable diseases increase alongside treatment innovations in medicine and pharmaceutical development. The cost-effectiveness estimates and HTA analyses are among some plausible solutions for making informed resource allocation decisions. The good work in those areas should make the health sector financing more sustainable and the significant system losses should shrink in the economic area.
Limitations of this review are the lack of numerical values expressed in the economic indicators (PPP, USD $, OOP) which could be compared with the results of the economic investigation from studies that dealt with subjects of healthcare expenditure and percentage of GDP investments. As this study is imagined as the descriptive study of current articles, the aim was to display all factors that directly and/or indirectly affected the global increase of healthcare expenditure. Summation of the factors that affect the healthcare expenditure could be useful for readers in designing a similar investigation in their countries considering all mentioned elements and maybe expanding investigation with quantitative economic indicators. The similarity of the results from articles considered in this review could be seen in Table 1 that implies the relationship between GDP and healthcare expenditure with each other and with different contributing factors.
LIST OF ABBREVIATIONS
| GDP | = Global Domestic Products |
| HCE | = Healthcare Expenditures |
| UHC | = Universal Health Coverage |
| OECD | = Organization for Economic Co-operation and Development (36 member countries) |
| BRICS | = Association of five major emerging national economies: Brazil, Russia, India, China, and South Africa |
| CEMAC | = Economic Community of Central African States |
| CIVETS | = Six emerging markets countries – Colombia, Indonesia, Vietnam, Egypt, Turkey, and South Africa |
| MENA | = Middle East and North Africa region |
| EM7 | = Seven countries that represent the largest Emerging Market countries – China, India, Brazil, Russia, Mexico, Indonesia, and Turkey |
| CIS | = Commonwealth of Independent States of 10 post-Soviet republics |
| SEE | = Southeast European Cooperative Initiative |
| AMA | = American Medical Association |
| ACA | = American Counseling Association |
| OOP | = Out of Pocket |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
Grant funded by Swedish FORTE number 2017-02235 and Grant OI 175014 funded by the Serbian Ministry of Education Science and Technological Development have jointly co-financed the underlying efforts behind this contribution.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Professor Mihajlo (Michael) Jakovljevic, Department of Global Health, Economics and Policy, Faculty of Medical Sciences, University of Kragujevac and Professor Ulf Gerdtham, Division of Health Economics, Lund University, Sweden have contributed to this article in an advisory capacity, while not fully fulfilling the ICMJE criteria for full authorship.




